Drug Development & Delivery - 09/2023
SPECIAL FEATURE – Injection Devices: Designing in Sustainability, Usability & Digitization for Patient Compliance
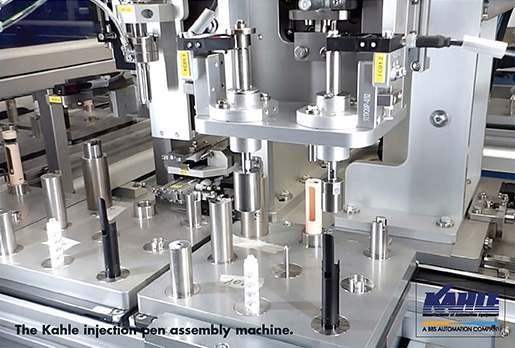
Reusable injection devices designed to accept prefilled syringes or drug cartridges are improving adherence and treatment outcomes through innovative designs. As these therapy-specific designs are developed, many utilize microcomponents with unique features requiring complex assembly. According to John Wuschner, Vice President Engineering at Kahle Automation, getting these designs from small batch to high-volume production quantities benefits from automation for three main reasons:
Efficient Speed: High volume by definition would make this reason obvious, but the assembly of injection devices requires more than just going faster, it requires a higher level of complexity. Feeding of the components without causing damage is critical here when one considers that disposable needle assemblies are produced at speeds of over 1,300ppm. Ensuring the sharp stays sharp and the functionality of the device is maintained all the way to the customer is challenging at these speeds. “Even the reusable pen injectors themselves with their intricate settable dosage dials have to be carefully threaded together at speeds of 400ppm,” says Mr. Wuschner.
Consistency: Automated processes are designed to mitigate the risks of assembly by having six-sigma process capability proven in advance of application to the line. By so doing, not only is the probability of rejects reduced, but also the key performance indicators of the product can be managed to generate results that perform equivalently lot to lot. Performance consistency in the device translates to shorter learning curves and leads to greater adherence by the patient, he says.
Quality: While process control is paramount, automated systems also benefit from an array of quality controls that can also be integrated at these high speeds. Needle tip geometry can be inspected through computer vision inspection of the tip, functional tests can be performed to ensure patency of the fluid path or proper actuation forces, and even cosmetic indicators can be used to verify that components were manufactured to critical specifications or that the proper components are being assembled in cases where one line produces several variants of a product family.
If identified, a rejected component (or partial assembly) can be segregated from further operations (reducing wasted components) and placed in a controlled container to avoid mixing rejects with valid product. Data can be automatically collected to identify where the defect occurred and cataloged by position, process, etc. to allow trending and data analysis to be performed. This aids root-cause analysis and helps prioritize the continuous improvement process for the line. Coupled with a SCADA system, this data can be automatically delivered to factory support personnel via production monitors and even triggered as alerts on smartphones based on thresholds customized by the user. Products can also be labeled or marked/tagged with lot control features during production or even serialized. In the event of a major non-conformance at later stages, these features allow for easier segregation of suspect product from valid product.
“These three motives for automation together form a foundation for efficient production of devices which, in concert with the device design, help enhance the patient experience through consistency and high reliability while also reducing the overall unit cost,” says Mr. Wuschner.
Article excerpt sourced from drug-dev.com, read the full article in: SPECIAL FEATURE – Injection Devices: Designing in Sustainability, Usability & Digitization for Patient Compliance